 |
 |
 |
 |
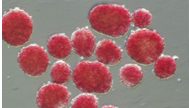
Diabetes is a serious disease, which, if not controlled, can be life threatening. It is often associated with long-term complications that can affect every system and part of the body. Diabetes can contribute to eye disorders and blindness, heart disease, stroke, kidney failure, amputation, and nerve damage. It can affect pregnancy and cause birth defects, as well. The most common form of diabetes is type 2 diabetes, which is a result of insulin resistance (a condition in which the body fails to properly use insulin), combined with relative insulin deficiency. Most Americans who are diagnosed with diabetes have type 2 diabetes. CITC is focused on research in the area of type 1 diabetes. Type 1 DiabetesType 1 diabetes results from the body's failure to produce insulin, the hormone that "unlocks" the cells of the body, allowing glucose to enter and fuel them.It is an autoimmune disease in which the body views the beta cells (insulin producing cells found in the islets of the pancreas) as a foreign substance, so the patient's immune system attacks the islets and kills them. It is estimated that 5-10% of Americans who are diagnosed with diabetes have type 1 diabetes. Most people with type 1 diabetes do not have a family history of the disease. We do not know how to prevent the onset of type 1 diabetes. Common Treatments for Type 1 DiabetesIntensive Insulin Therapy Insulin may be taken by means of a shot (often several times a day), or infused through catheter (a small needle) attached to an insulin pump. Recently an inhalable insulin has been approved by the FDA. It is important for anyone with diabetes to be careful about the type, timing and amount of food they eat. People with diabetes also need to monitor their bloodsugars carefully through frequent finger prick glucose testing. A person with diabetes may experience long term complications if tight blood sugar control is not maintained; likewise, control that is too tight may result in severe hypoglycemic (low blood sugar) reactions. Pancreas Transplant Islet Transplantation and Other Experimental Treatment Options Lastly, it is important to note that individuals that receive a pancreas or islet transplant must take immunosuppressive medications as long as the pancreas or islets are functioning. The risks and benefits of either procedure are complex and are not limited to the issues discussed in this brief summary. Islet transplantation is described in other sections of this website. You may also find links to interesting research being conducted in the field of type 1 diabetes by visiting our Links page.
|
| Home | |

|